Introduction
I'm Chris Uhlik, age 64½. I've always thought of myself as a pretty healthy guy. I exercise moderately, I'm relatively active, and I eat well, never smoked, barely ever drink any alcohol, etc. While I can get intensely focused at times, I think I'm pretty relaxed and low-stress. But I also have a family history of early onset CAD. It turns out that if your genetics predispose you to this, no amount of exercise or healthy living is going to buy you more than a couple more years. This is the story about how I found out I have severe corenary artery disease and how I am getting through a heart bypass operation (Two Vessel CABG).
I'm sharing this for a few reasons:
- To augment my own memories
- To help my friends and family recognize symptoms if they have something similar
- To encourage you to do significant testing beyond the occasional blood lipid panel
- To make up for my inability to keep everyone up to date appropriately --- I'm just not a social media guy and don't know how to tap heart-felt messages out to dozens of friends and family when I'm tired and sore.
I hope you learn something useful, enjoy sharing the experience, and maybe, just maybe somebody will avoid a heart attack because of something they learned while reading my story.
March 28 Crashes in Baja
 I didn't know it at the time, but in retrospect, this explanation fits. A couple of times
riding with JB Carillo, Armando Nuza, and friends,
I lost control of the bike and crashed inexplicably. Both
were in strenuous situations (whoops and lots of tight
turns) where "something happened" and I just sort of
turned off and failed to control the bike in a situation
where, normally I would have had no problem. At the time,
I chalked it up to pushing too hard, but I think I might
have run into a markedly reduced cardiovascular limit.
I didn't know it at the time, but in retrospect, this explanation fits. A couple of times
riding with JB Carillo, Armando Nuza, and friends,
I lost control of the bike and crashed inexplicably. Both
were in strenuous situations (whoops and lots of tight
turns) where "something happened" and I just sort of
turned off and failed to control the bike in a situation
where, normally I would have had no problem. At the time,
I chalked it up to pushing too hard, but I think I might
have run into a markedly reduced cardiovascular limit.
 A couple of days earlier, during a particularly difficult run
across the desert towards San Filipe in deep sand, I found myself
exhausted and stopping to rest a lot, well behind the rest of the group. I didn't crash, but I wasn't feeling up to my "full strength".
A couple of days earlier, during a particularly difficult run
across the desert towards San Filipe in deep sand, I found myself
exhausted and stopping to rest a lot, well behind the rest of the group. I didn't crash, but I wasn't feeling up to my "full strength".
April 5 Walking around Milan
 While Kathi and I were doing our typical 20k steps wandering the city, I found myself
occasionally a little uncomfortable walking around the city (flat ground). At the time I chalked it up to jet-lag.
Pausing to rest made the discomfort go away immediately. I thought nothing of it.
While Kathi and I were doing our typical 20k steps wandering the city, I found myself
occasionally a little uncomfortable walking around the city (flat ground). At the time I chalked it up to jet-lag.
Pausing to rest made the discomfort go away immediately. I thought nothing of it.
April 7 Walking in Malta at night
 Here's where it gets serious...
The first real event was our first night in Malta (Apr 7)
walking back from Marsaskala Harbor to Mulberries (about 2.3km and
maybe 70m elevation gain) after dinner at about 9:30pm. I was feeling
weird pains in the elbow joints and my armpits and my esophagus. When
I stopped walking and rested for about a minute, the pain would go
away. I was not short on breath, but my chest hurt. This forced me
to stop and rest at least 5 times over a stretch of about 1 km where
the slope was perhaps 5%, uphill for sure, but not steep.
Here's where it gets serious...
The first real event was our first night in Malta (Apr 7)
walking back from Marsaskala Harbor to Mulberries (about 2.3km and
maybe 70m elevation gain) after dinner at about 9:30pm. I was feeling
weird pains in the elbow joints and my armpits and my esophagus. When
I stopped walking and rested for about a minute, the pain would go
away. I was not short on breath, but my chest hurt. This forced me
to stop and rest at least 5 times over a stretch of about 1 km where
the slope was perhaps 5%, uphill for sure, but not steep.

This was a pretty scary event as it was very dark and we were quite far from anything familiar. I didn't even know the local "911" phone number! But it didn't feel serious. It was just weird pain in my elbows and an irresistable urge to raise my arms over my head and roll my shoulders. I'm glad I didn't panic and the problem eased quickly if I just paused and rested for 20 seconds.
Over the next several days in Malta, this pattern repeated maybe 4 more times where walking after dinner would cause chest and arm discomfort. We (Kathi and I) thought it might be an esophageal reflux issue after eating a big meal, but it happened after small meals and once mid-day several hours after a light breakfast.
April 14--21 Sicily
Over the next 3 weeks, walking around Sicily, Rome, and Florence, it happened a little bit more. I was more ready to just stop and rest at the first signs of pain. It did not again become as severe as the first time in Malta.
We flew to Sicily, and walking around A LOT, I don't remember any issues at all during our stay in Sicily.
April 22--26 Rome
We flew to Rome, spent a day with Kathi sick in bed, then walked around A LOT. I do remember some periods of mild chest and elbow discomfort during our walks in Rome, but at this point I was taking it in stride; just pausing to rest when it became annoying. It really didn't get in our way. If anything, it slowed Chris down to a pace more comfortable for Kathi. I was just taking it easy and enjoying Italy.
April 28--May 2 Italian Classes in Firenze
I don't remember any issues walking around Firenze. However, one evening in our apartment in Firenze Chris was feeling a super slow heartbeat. I was getting ready for bed and my heart was doing something funny. My heart rate was about 50 bpm, but for extended periods it would skip every other beat, so something like 25 bpm. Unnerving, but what can you do? So I went to sleep and it was fine in the morning.
May 5--9 Italian Classes in Via Reggio
I don't remember any issues walking around Via Reggio.
May 12 Scooter to Corsica
Remarkably, while riding around Corsica for a week, I had zero issues. But, remember I was riding by myself in a very unfamiliar area, so I was being quite conservative, enjoying the view, and not really exerting myself much.
May 17--20 Scooter riding in Sardenia
Again, while riding around Sardenia for a week, I had almost zero issues, until...
May 19 Scooter Stuck in Sardenia
Over the 2 weeks of riding in Corsica and Sardenia (May 11--20) I had no problems except maybe a tiny bit once when I was a bit paniced about getting my bike stuck in a ditch in the middle of nowhere. I rested and got the bike out without too much pain, but in retrospect I think I was feeling chest issues then too. It's interesting that in all that extensive motorcycle riding, which is non-trivial exertion, I did not experience any issues except for that one incident.

Sorry I don't have any pictures of the actual event. There were incredible meadows of wildflowers up in the remote areas of Sardenia. I stopped to park my scooter in a meadow for a picture, but the bike sunk into a rut and got stuck. I hadn't seen another person in over an hour and wasn't feeling strong at altitude. I think I might not have been thinking clearly either, so no pictures. But, really it did happen, ..., really ;-)
By taking it a little bit at a time, and resting frequently, I managed to get the bike back on the road, but my heart was pounding the whole time.
May 22 Flying to Germany
Our time in Italy comes to a close. Kathi and I rejoin in Milan, then fly to Frankfurt and make our way to Laudenberg, Germany, where we would meet up with my brother Joe (and wife Bridget) who lives there and my brother Matt who flew in from California with my mother. Mini reunion time with Mom and her 3 sons.
May 24 Feeling it again walking around Germany
In Germany with Kathi, Joe, Matt, Mom, and Bridgett, I had very slight pains a couple of times.
May 29 Flying back to The States
We flew back to PDX without incident and I forgot about chest pains for a couple of months.
June 7 WTF? another stupid crash!
 Shortly after returning to the USA, June 7,
riding my CRF450L in Waddell
in Northern Washington, I had a crash which I didn't attribute to this
heart issue at the time, but in retrospect seems quite similar to my March Baja
experience where I'm riding pretty hard and then just fall for no particular reason.
I got lucky and just bashed my knee into soft dirt. I think the cause was running
into my aerobic capacity limit and having more of a brain control failure without
any warning angina pain; that being masked by the adrenaline of hard dirt riding.
Shortly after returning to the USA, June 7,
riding my CRF450L in Waddell
in Northern Washington, I had a crash which I didn't attribute to this
heart issue at the time, but in retrospect seems quite similar to my March Baja
experience where I'm riding pretty hard and then just fall for no particular reason.
I got lucky and just bashed my knee into soft dirt. I think the cause was running
into my aerobic capacity limit and having more of a brain control failure without
any warning angina pain; that being masked by the adrenaline of hard dirt riding.

June 22--28 Scooter Cannonball
 Later in June 21--29, I rode the endurance Scooter Cannonball without incident.
Even though the days were long and full of mild exertion for 12+ hours at a time,
I think any symptoms were masked by adrenaline.
Later in June 21--29, I rode the endurance Scooter Cannonball without incident.
Even though the days were long and full of mild exertion for 12+ hours at a time,
I think any symptoms were masked by adrenaline.
July and August
So, after coming back to the USA, I mostly forgot about this until several times in the evening when I was dragging trash cans out to the curb, I would get the elbow and chest pain briefly. Once after that I checked my blood pressure and it was suprisingly high --- don't remember the exact numbers but something like 180/110. My heart rate was not high and the blood pressure returned to normal quickly.
One time in the evening, I don't remember when (it might have been in June or July), I experienced a pounding heart (very strong heartbeat) and highly irregular heart rate where I had many missed beats. That lasted maybe 5 minutes before I fell asleep.
Dragging out the trash cans
 Beginning around the end of August, I had something repeatable. Every Tuesday
evening, while dragging the trash cans up the driveway to the gate, I'd get those
darn elbow pains, rolly shoulders, and tightness in my sternum. I'd push though
for the 2 minutes it took to position the cans at the curb, then walk back, and
typically the pain would have subsided before I even made it back to the couch.
Beginning around the end of August, I had something repeatable. Every Tuesday
evening, while dragging the trash cans up the driveway to the gate, I'd get those
darn elbow pains, rolly shoulders, and tightness in my sternum. I'd push though
for the 2 minutes it took to position the cans at the curb, then walk back, and
typically the pain would have subsided before I even made it back to the couch.
Is there a pattern?
I looked for a pattern. Was it right after a meal? Not always. Sometimes 3 hours after eating I'd get the same thing. Then a few weeks later, I'd have a pain for a few seconds just sitting on the couch --- no trash cans required. Well, my annual physical should be coming up. I think I should schedule a conversation with Dr. Dela Cruz, my family doctor.
Dr. Dela Cruz physical
 I called Kaiser to schedule a physical exam and had a
conversation with the scheduler. They asked lots of
questions, then got a cardiologist on the line where I
went though the questions again. They decided I was
stable, but expedited my appointment with Dela Cruz. At
the appointment, they collected a resting EKG, did the
typical height and weight and blood pressure measurements,
listened to my heart and lungs, gave me my Flu and Covid
vaccinations, and crucially, ordered a cardiac stress test
(EKG while walking on a treadmill). It would be 5 weeks
waiting for the stress test.
I called Kaiser to schedule a physical exam and had a
conversation with the scheduler. They asked lots of
questions, then got a cardiologist on the line where I
went though the questions again. They decided I was
stable, but expedited my appointment with Dela Cruz. At
the appointment, they collected a resting EKG, did the
typical height and weight and blood pressure measurements,
listened to my heart and lungs, gave me my Flu and Covid
vaccinations, and crucially, ordered a cardiac stress test
(EKG while walking on a treadmill). It would be 5 weeks
waiting for the stress test.
I got to carry the EKG printout from the imaging lab to my doctor, so I grabbed a picture. My heart rate is a little low at 57 bpm (sinus bradycardia) and there's a small "Nonspecific T wave abnormality". This would not be considered important until after the cardiac stress test.
Road trip to see our California Friends
 While waiting the month between
my physical and my cardiac stress test, Kathi and I did
our annual drive to the SF Bay Area to see her sisters and
our Stanford and Google friends. We had a wonderful party
at Rob and Julie's place. The next day Mike and Celia
organized a walk at Foothills Park. I walked with Mike
and Celia while Kathi was ahead walking with Fred. During
that Sunday morning hike in Foothills Park, I had a
relatively intense episode, but I knew how to slow down
and manage the feeling. The whole thing made some super
interesting conversation. At this age, a surprising
number of my friends have had health events, and you don't
really hear about this stuff until you "join the club".
It turns out one of my friends recently had an actual
Myocardial Infarction (heart attack where some heart
muscle is injured by lack of oxygen). He had an emergency
angiogram and had a stent placed in his LAD. As you can
imagine, a lot of the talk during that week was about
chest pains and the various testing options available. I
had a cardiac stress test already scheduled, but also
decided I might get a Cardiac CAC CAT scan next week while
Kathi and I were visiting Nicky in Las Vegas. That CAC
test uses a 3D X-Ray CAT scan to measure calcium deposits
in coronary arteries. For men anyway, the arterial
plaques tend to be calcified and can be detected this way.
I resolved to get a cash-out-of-pocket CAC scan at Desert
Radiology while in Vegas next week. Bringing that data to
my stress test couldn't hurt and I was getting damn
curious.
While waiting the month between
my physical and my cardiac stress test, Kathi and I did
our annual drive to the SF Bay Area to see her sisters and
our Stanford and Google friends. We had a wonderful party
at Rob and Julie's place. The next day Mike and Celia
organized a walk at Foothills Park. I walked with Mike
and Celia while Kathi was ahead walking with Fred. During
that Sunday morning hike in Foothills Park, I had a
relatively intense episode, but I knew how to slow down
and manage the feeling. The whole thing made some super
interesting conversation. At this age, a surprising
number of my friends have had health events, and you don't
really hear about this stuff until you "join the club".
It turns out one of my friends recently had an actual
Myocardial Infarction (heart attack where some heart
muscle is injured by lack of oxygen). He had an emergency
angiogram and had a stent placed in his LAD. As you can
imagine, a lot of the talk during that week was about
chest pains and the various testing options available. I
had a cardiac stress test already scheduled, but also
decided I might get a Cardiac CAC CAT scan next week while
Kathi and I were visiting Nicky in Las Vegas. That CAC
test uses a 3D X-Ray CAT scan to measure calcium deposits
in coronary arteries. For men anyway, the arterial
plaques tend to be calcified and can be detected this way.
I resolved to get a cash-out-of-pocket CAC scan at Desert
Radiology while in Vegas next week. Bringing that data to
my stress test couldn't hurt and I was getting damn
curious.

Chris, Mike, Fred, Celia, Kathi

The lovely Kathi who managed to get up for an early morning hike, thank-you KB.
Lithia Park Hike
 On the drive back north, we often stop to walk around Lithia Park
in Ashland Oregon. During our very calm, careful walk, I had the feeling come and go a
couple of times with super light exertion. Then suddenly it went away and I could walk
briskly with no issue. This is so weird!
On the drive back north, we often stop to walk around Lithia Park
in Ashland Oregon. During our very calm, careful walk, I had the feeling come and go a
couple of times with super light exertion. Then suddenly it went away and I could walk
briskly with no issue. This is so weird!
Las Vegas, Red Rock
 While visiting Nicky and Olivier
in Las Vegas to watch her perform in Vegas Variety Circus,
Kathi and I went for a couple of walks in Red Rock. Once
just Kathi and I but another time with our friend Ana Liu.
Both times, I had to modulate my pace to control chest
pains.
While visiting Nicky and Olivier
in Las Vegas to watch her perform in Vegas Variety Circus,
Kathi and I went for a couple of walks in Red Rock. Once
just Kathi and I but another time with our friend Ana Liu.
Both times, I had to modulate my pace to control chest
pains.
Cardiac Stress Test
 Treadmill stress test in Salem.
On Nov 6 I drove to Salem in the afternoon where I was
hooked up to a 12-lead EKG and subjected to
the Bruce Protocol on a treadmill under
the supervision of a nurse. I made it through levels 1--4
(16% grade, 4.2 mph) but gave up with strong arm and
angina pain just before the transition to level 5.
Treadmill stress test in Salem.
On Nov 6 I drove to Salem in the afternoon where I was
hooked up to a 12-lead EKG and subjected to
the Bruce Protocol on a treadmill under
the supervision of a nurse. I made it through levels 1--4
(16% grade, 4.2 mph) but gave up with strong arm and
angina pain just before the transition to level 5.
Results - EKG 12 OR MORE LEADS W INT & RPT - Final result (11/07/2025 11:10 AM PST)
Authorizing Provider: Amor Dela Cruz, MD Result Type Result Status: EKG Final Result
STRESS TEST ONLY, EXERCISE WO PHYSICIAN SUPERVISION, CV (11/06/2025 2:25 PM PST)
Results - STRESS TEST ONLY, EXERCISE WO PHYSICIAN SUPERVISION, CV (11/06/2025 2:25 PM PST)
Component Value
------------------------------ ---------
Stress protocol BRUCE
Time in exercise phase 11m56s
Estimated workload, post stress 13.4 METS
Maximum Systolic, BP 180 mmHg
Maximum Diastolic BP 96 mmHg
Peak heart rate, stress 164 bpm
Baseline heart rate, stress 65 bpm
Baseline BP, Stress 118/84 mmHg
Target Heart Rate Reached, Stress 1
Final HR 82 bpm
Peak Final Systolic BP 164 mmHg
Peak Final Diastolic BP 93 mmHg
Reason for termination See EPIC
Target heart rate, stress 133 bpm
% target HR 123.68 %
Maximum heart rate % 105.13 %
Stress % predicted METS 174.93 %
Resting SPO2 98
Peak exercise SPO2 97
Stress predicted METS 7.7 METS
Exercise duration, post stress 11m56s
Rate pressure product 26,896.0
Heart rate recovery, minute 1, stress 127 bpm
Heart rate recovery, minute 2, stress 87 bpm
Peak BP, post stress 164/94 mmHg
Results - STRESS TEST ONLY, EXERCISE WO PHYSICIAN SUPERVISION, CV (11/06/2025 2:25 PM PST)
Anatomical Region Laterality Modality Other
Results - STRESS TEST ONLY, EXERCISE WO PHYSICIAN SUPERVISION, CV (11/06/2025 2:25 PM PST)
Specimen (Source) Anatomical Location / Laterality Collection Method / Volume Collection Time Received Time
11/06/2025 2:24 PM PST
Results - STRESS TEST ONLY, EXERCISE WO PHYSICIAN SUPERVISION, CV (11/06/2025 2:25 PM PST)
Narrative
11/06/2025 2:28 PM PST
This result has an attachment that is not available.
• Procedure details: A Bruce protocol stress test was performed. Overall,
the patient's exercise capacity was above average for their age. The
patient reached stage 4 of the protocol after exercising for 11 min and 56
sec and had a maximal HR of 164 bpm (105.13% of MPHR) and peak METS of
13.4. The patient experienced no angina during the test. The test was
stopped because the patient experienced fatigue and atypical chest pain
and bilateral arm pain. Resting BP was normal with a hypertensive response
to stress. Heart rate demonstrated a normal response to stress. The
patient's heart rate recovery was normal. The one minute heart rate
recovery was 127 bpm. The two minute heart rate recovery was 87 bpm.
• Stress ECG: No ST deviation or T wave abnormalities was noted. There
were no arrhythmias during stress. There were no arrhythmias during
recovery.
• Resting ECG: The ECG shows normal sinus rhythm.
• ECG Conclusion: The ECG was negative for ischemia.
Achieving > 10 METs confers a very low risk of cardiac events in the near term
(<1% risk of having significant ischemia, 0.1% risk of cardiac death per year, <1% risk of MI per year).
Results - STRESS TEST ONLY, EXERCISE WO PHYSICIAN SUPERVISION, CV (11/06/2025 2:25 PM PST)
Authorizing Provider Result Type Result Status
Amor Dela Cruz, MD CV STRESS PROCEDURES Final Result
Whoopee! I'm in the clear. Normal EKG, <1% risk of having a heart attack. Yay, I can get back to exercising. This doesn't look like a heart issue...
Cardioligist reads the Stress Test EKG
 So, the day after the stress
test, I have an appointment with Dr. Olga V Demina, DO, a
bonafide Cardiologist who will counsel me on the results.
She asked me, "So what do you think about your stress
test?" I express my happiness that it doesn't look like
I'm about to have a heart attack, I can get back to
exercising, and by-the-way, what's the next step for
investigating these chest and arm pains, because something
is still going on, even it if isn't my heart...
So, the day after the stress
test, I have an appointment with Dr. Olga V Demina, DO, a
bonafide Cardiologist who will counsel me on the results.
She asked me, "So what do you think about your stress
test?" I express my happiness that it doesn't look like
I'm about to have a heart attack, I can get back to
exercising, and by-the-way, what's the next step for
investigating these chest and arm pains, because something
is still going on, even it if isn't my heart...
Olga says, "I see that you might know something about signal processing, let me explain these EKG results to you." She then goes on to point to various sections of the waveform saying things like "I don't like how this is going down here. It should be rising or at least flat, not down. This is very concerning. I think you have blockage in your LAD (Left Anterior Descending coronary artery). I want you to go in for an invasive angiogram with contrast dye as soon as possible. I'm going to have them call you sometime today or tomorrow to schedule the procedure." At first I'm stunned. WTF? how could the stress test nurse have gotten the narative so wrong. Crap, I could have died on that treadmill! Well, at least I'm lucky to find this early and they are taking it seriously. We are going to get to the bottom of this. Maybe I'll come out of my angiogram with a stent and be back to 100% in no time.
A note about my Cardiologist. Dr. Olga V Demina, DO, Cardiologist studied at Midwestern University Chicago College of Osteopathic Medicine; Fellowship: Rush University Medical Center, Chicago; Residency: Advocate Lutheran General Hospital, Park Ridge, IL; joined Kaiser 2025; she looks like she's 20 years old. But despite her apparent inexperience, had a really engaging bedside manner. Encouraged me to talk about the cardiac stress test and how I felt about the result before tactfully telling me the findings in the narrative were wrong and why and how serious it was to get moving on next steps. She said it is very likely I will be in for at least a stent and possibly bypass surgery. And sure enough, she got the ball rolling a lot faster. Kaiser called me back later that day to schedule a cardiac echo (ultrasound) and the angiogram. The echo would be done early next week. The angiogram slots were booked out until next year, except for one opening the day before Thanksgiving. I'll take it.
* We're going to plan for a cardiac catheterization to further assess your chest pain.
* While you are awaiting cardiac cath we will start you on amlodipine (2.5 mg) to dilate blood vessels and
rosuvastatin (5 mg) (cholesterol lowering medication).
* Please change aspirin from 325 mg to 81 mg daily.
* Nitroglycerin (NITROSTAT/NITROTAB) 0.4 mg dissolve under tongue as needed for chest pain.
May repeat 2 times at 5 minute intervals. Call 911 if pain persists
* If your symptoms get worse worse or more frequent go to the ER- call 911 do NOT
drive yourself there.
Ordered:
* CARDIAC CATHETERIZATION: LEFT
* BASIC METABOLIC PANEL
* CBC (COMPLETE BLOOD COUNT)
* TRANSTHORACIC ECHO
Today's visit:
* BP 136/83 57 bpm O2-sat 98%
* Weight 171 lbs, BMI 25.25
Good Grief, I must be getting old. I'm on heart meds now!
Echocardiogram (Cardiac Ultrasound measurements)
 A "TRANSTHORACIC
ECHO (TTE) COMPLETE W STRAIN AND CONTRAST" is an
interesting ultrasonic imaging protocol where they inject
agitated saline with microscopic bubbles via an IV and the
bubbles reflect ultrasound making blood more visible /
contrasty.
A "TRANSTHORACIC
ECHO (TTE) COMPLETE W STRAIN AND CONTRAST" is an
interesting ultrasonic imaging protocol where they inject
agitated saline with microscopic bubbles via an IV and the
bubbles reflect ultrasound making blood more visible /
contrasty.
They measure diameters and cross-sectional areas of various chambers, veins, and arteries. They measure "ejection fraction" what fraction of the heart's volume is pumped per cycle. And they look carefully at the conditions of each of the heart valves. The images are impressively clear, and they have doppler which measures some blood flow information, but only at a gross level. I was surprised that they could not see blood flowing in the LAD artery. It seems that small movement of blood in smaller arteries is drowned out by the overall movement of the heart muscle.
Overall, their goal is to evaluate the sqeezing functionality of the heart muscle and how effectively the heart is pumping.
TRANSTHORACIC ECHO (TTE) COMPLETE W STRAIN AND CONTRAST, CV (11/11/2025 12:18 PM PST)
Results - TRANSTHORACIC ECHO (TTE) COMPLETE W STRAIN AND CONTRAST, CV (11/11/2025 12:18 PM PST)
Component Value
BSA, DUBOIS 1.931
ASCENDING AORTA DIAMETER 3.00 cm
AORTIC ROOT DIAMETER 3.00 cm
LEFT VENTRICULAR DIASTOLIC SEPTAL THICKNESS 0.68 cm
LVOT mean vel 0.70 cm/s
Aortic valve mean velocity 1.00 m/s
LVOT peak gradient, at rest 4 mmHg
Left ventricular cardiac output 2.91 l/min
Aortic sinus of Valsalva diameter 3.0 cm
Right atrial volume, 2D 40.0 mL
EDV A4C 7.95 mL
Left ventricul diastol area, endocard, parastern short axis view 30.50 cm2
Left ventricular posterior wall thickness in end diastole 0.67 cm
Left ventricular area endocard in systole, parastern short axis 17.90 cm2
Right atrial area in systole, apical 4 chamber view 13.9 cm2
Tricuspid valve peak velocity regurgitant flow 2.1 m/s
Tricuspid annular plane excursion, systole 1.80 cm
Mitral valve area, PHT 64 ms
Mitral valve peak gradient 3 mmHg
Mitral valve peak E velocity 0.81 m/s
Mitral valve peak A velocity 0.74 m/s
Mitral valve E' tissue velocity, septal 0.09 m/s
Mitral valve E' tissue velocity, lateral 0.11 m/s
Mitral valve deceleration time 219 ms
Left ventricular outflow tract VTI 19.70 cm
Left ventricular outflow tract peak velocity 0.98 m/s
Left ventricular outflow tract mean gradient 2 mmHg
Left ventricular outflow tract diameter 1.8 cm
Left ventricular posterior wall thickness, end diastole 0.67 cm
Left ventricular mass size 1 78.59
Left ventricular internal dimension, systole 2.4 cm
Left ventricular internal dimension, diastole 4.1 cm
Left ventricular end volume, systole, biplane method of disks 44.50 mL
Left ventricular end volume, systole, 3D 39.0 cm3
Left ventricular volume, end diastole, biplane method of disks 104.00 mL
Left ventricular volume, end diastole, 3D 86.0 cm3
Left atrial volume, biplane method of disks 40.1 mL
Left atrial size 3.2 cm
Left atrial area, apical 4 chamber, systole 14.90 cm2
Interventricular septum thickness, end diastole 0.7 cm
Inferior vena cava point-to-point dimension 1.2 cm
AV peak gradient 10 mmHg
Ascending aorta point-to-point dimension 3.0 cm
Aortic valve VTI 30.40 cm
Aortic valve peak velocity 1.62 m/s
Aortic valve mean gradient 5 mmHg
Aortic sinus point-to-point dimension 3.0 cm
Aortic valve area peak velocity 1.5 cm2
Aortic valve area VTI 1.6 cm2
Aortic valve area index 0.9 cm2/m2
Ejection fraction, 3D 55 %
Ejection fraction, biplane 57 %
Fractional shortening 41 %
Left atrium to aorta ratio 1.07
Left atrial volume index, biplane method of disks, BSA 20.8 mL/m2
Left ventricular relative wall thickness, 2D 0.33 cm
Left ventricular outflow tract area 2.54 cm2
Left ventricular outflow tract stroke index 25.96 ml/m2
Left ventricular outflow tract stroke volume 59.50 cm3
Mitral valve area pressure half time 3.44 cm2
Mitral valve E/A ratio 1.09
Mitral valve E/e' ratio 8.18
Tricuspid valve peak gradient regurgitant flow 18 mmHg
Left ventricular internal dimension at end systole index, BSA 1.2 cm/m2
Right atrium end systolic volume index, BSA,apical 4 chamber view 20.7 mL/m2
Left ventricular end diastolic volume index, 3D, BSA 44.56 cm3/m2
Left ventricular end systolic volume index, 3D, BSA 20.21 cm3/m2
Mitral valve E/e' tissue velocity, lateral 7.36 m/s
Left ventricul end systol volume index, biplane meth of disks,BSA 23.1 mL/m2
Left ventricul end diastol volume index,biplane meth of disks,BSA 53.9 mL/m2
Left ventricular end diastolic volume index, 2D, Teichholz, BSA 38.46 ml/m2
Left ventricular end systolic volume index, 2D, Teichholz, BSA 10.45 ml/m2
Left ventricular end diastolic volume, 2D, Teichholz formula 74.22 mL
Left ventricular end systolic volume, 2D, Teichholz formula 20.16 mL
Left ventricular diastolic internal dimension index, BSA 2.1 cm/m2
Aortic valve velocity ratio, peak velocity 0.60
Mitral valve E/e' tissue velocity, septal 9.00 m/s
Aortic valve velocity ratio, VTI 0.65
Left ventricular mass index, 2D 41.15 g/m2
Mitral valve area index, BSA 1.78 cm2/m2
Left ventricular mass, 2D 79.43 g
Asc Ao Z-score -2.17
SoV Z-score -2.83
LVEF, Teicholz 73 %
SoV Index 1.55 cm/m2
Asc Ao Index 1.55 cm/m2
Estimat RVSP 21 mmHg
Right atrial pressure, estimated 3 mmHg
Pulmonary artery pressure, systole 21 mmHg
Global longitudinal strain -19.8 %
Narrative
11/12/2025 3:14 PM PST
This result has an attachment that is not available.
• Left Ventricle: Ultrasound enhancement agent used for improved
visualization. Left ventricle size is normal. Normal wall thickness. No
thrombus present in the left ventricle. Normal systolic function with an
estimated EF of 55 - 60%. EF by 2D Simpson biplane is 57%. EF by 3D
resconstruction is 55%. Global longitudinal strain is normal (GLS -19.8%).
Regional wall motion abnormalities present. Subtle hypokinesis of the
apical lateral segment.
• Right Ventricle: Right ventricle size is normal. Normal systolic
function. TAPSE is 1.80 cm.
• No significant valvular abnormalities.
Left Ventricle
Ultrasound enhancement agent used for improved visualization. Left ventricle size is normal. Normal wall thickness. No thrombus present in the left ventricle. Normal systolic function
with an estimated EF of 55 - 60%. EF by 2D Simpson biplane is 57%. EF by 3D resconstruction is 55%. Global longitudinal strain is normal (GLS -19.8%). Regional wall motion abnormalities
present. Normal diastolic function.
Right Ventricle
Right ventricle size is normal. Normal systolic function. TAPSE is 1.80 cm.
Left Atrium
Left atrium size is normal. Left atrium volume index is 21 mL/m2. No evidence of interatrial shunt by color Doppler.
Right Atrium
Right atrium size is normal. RA volume index is 21 mL/m2.
IVC/SVC
Normal (<2.1 cm) IVC size with greater than 50% collapse, estimated right atrial pressure of 3 mmHg (normal).
Mitral Valve
Mitral valve structure is normal. Trace mitral regurgitation. No mitral stenosis.
Tricuspid Valve
Tricuspid valve structure is normal. Trace tricuspid regurgitation. The PASP is estimated to be 21 mmHg which is normal. No tricuspid stenosis.
Aortic Valve
Trileaflet aortic valve structure. No aortic regurgitation. No aortic stenosis.
Pulmonic Valve
Pulmonic valve structure is normal. Trace pulmonic regurgitation. No pulmonic stenosis.
Ascending Aorta
Normal sized sinus of Valsalva (aortic root) and ascending aorta.
Pericardium
No pericardial effusion.
Study Details
A complete echo was performed using 2D, spectral Doppler, and color flow and strain imaging. The apical, parasternal, subcostal,
and suprasternal views were obtained. Imaging was done using Definity ultrasound enhancing agent. Patient exhibited sinus rhythm. Study quality was good.
Prior Study
No prior study available for comparison.
Wall Scoring Baseline
Score Index: 1.06
The following segments are hypokinetic: apical lateral.
All other segments are normal.
Results - TRANSTHORACIC ECHO (TTE) COMPLETE W STRAIN AND CONTRAST, CV (11/11/2025 12:18 PM PST)
Authorizing Provider Result Type Result Status
Olga V. Demina, DO CV ECHO PROCEDURES Final Result
Olga's comments: "Your echocardiogram shows normal squeezing function of the heart. There were no issues with heart valves. Overall reassurance study."
So my ultrasound looks pretty good. Maybe a little loss of squeezing function in the left ventrical, but otherwise my squeezing is good, ejection fraction is good, and my valves are in good shape. And I really enjoyed the procedure. My technician was great and really shared the monitor and explained everthing she was doing.
While I'm there, they collected blood for a Basic Metabolic Panel and CBC Complete Blood Count.
Pre-Thanksgiving Invasive Angiogram
 I got up early to drive myself
1/2 hour south to Sunnyside Oregon for my surgery. I
needed to check in at 6:30am and the procedure was to take
up to 3 hours followed by anesthesia recovery. I tried to
park the car and send info to Kathi in case I had
post-anesthesia amnesia.
I got up early to drive myself
1/2 hour south to Sunnyside Oregon for my surgery. I
needed to check in at 6:30am and the procedure was to take
up to 3 hours followed by anesthesia recovery. I tried to
park the car and send info to Kathi in case I had
post-anesthesia amnesia.
I woke up around 10:30am and Kathi was there. My doctor asked me if I remembered our conversation after the surgery but I had zero memory. My conciousness was perfectly spliced from looking at the X-ray panel over the bed to looking at Kathi. Somehow, it didn't bother me at all that the X-ray panel had turned into a beautiful Kathi!
Anyway, here are the results:
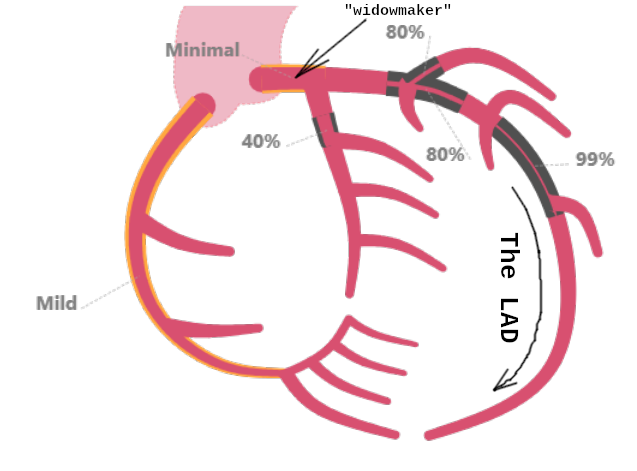
Conclusion
Right dominant coronary arteries with single vessel obstructive CAD manifested as a long, chronic occlusion in the mid LAD
LVEDP 10mmHg
Deflate TR band per protocol
Continue optimal medical therapy
Will discuss revasc options with patient. Stenting is probably feasible but would require ~80mm of stent and thus not be
expected to be a durable option
Pre Procedure Diagnosis
Angina with equiovocal stress testing
Post Procedure Diagnosis
1 vessel obstructive CAD
Indications
CHEST PAIN [R07.9 (ICD-10-CM)]
ABNL CARDIOVASCULAR STRESS TEST [R94.39 (ICD-10-CM)]
Procedures
CORONARY ANGIOGRAPHY
CARDIAC CATHETERIZATION LEFT HEART
Procedure Details
Cath Procedure Accessed site(s): right radial artery.
Details Ultrasound guided vascular access was used.
Catheter details: Tiger JR4
Pigtail
Sheath(s): 6 Fr.
Closure method(s): TR Band.
Hemostasis obtained.
Left Heart
Left Ventricle LV end diastolic pressure is normal. LVEDP: 10 mmHg.
Left Main
The vessel is long, large in caliber and has minimal luminal irregularities.
Left Anterior Descending
Prox LAD to Mid LAD is stenosed with 80% stenosed side branch in 1st Diag and 80.
Mid LAD is stenosed.
Left Circumflex
The vessel is moderate in caliber.
Prox Cx is stenosed.
Right Coronary Artery
The vessel is moderate in caliber and has mild disease throughout.
No complications were associated with this study.
The bad news.
Supplies
Name ID Tmp Type Qty
GUIDEWIRE VASC .035IN 260CM 3MM RDS J CRV TAPER STRT PTFE 3 130 No VASC CATH 1
277 GUIDE
BAND COMPRESS REG RADIUS TR BAND 24CM 2 BALLOON AIR INJ PORT 181 No Vascular 1
VELCRO STRAP INFLATR SYRINGE 333
PACK CUSTOM CARDIAC CVL SMC 253 No Packs 1
286
CATHETER ANGIO RADIALTIGER CRV 5FR 4MM 110CM CORONARY 1 257 No VASC Cath 1
SIDEHOLE DX OPTITORQUE 684
CATHETER ANGIO PIGTAIL 145 CRV 5FR .045IN 110CM VENTRICULAR 263 No VASC Cath 1
EXPO 08526-41 BX/5 861
CATHETER ANGIO .038IN JR4 CRV STD 5FR 100CM THRULUMEN DESIGN 266 No VASC Cath 1
GW VESTAN INFINITI 321
KIT INTRO 10CM 6FR 20GA GLIDESHEATH SLENDER .025IN 32MM SHORT 268 No VASC Cath 1
ANGLE PLASTIC HYDROPHILIC 119
Anesthesia Type
Procedure
CORONARY ANGIOGRAPHY Procedural Sedation
CARDIAC CATHETERIZATION LEFT HEART Procedural Sedation
Midazolam Inj (VERSED) (mg) Total dose: 1.5 mg
Date/Time Rate/Dose/Volume Action
fentaNYL (PF) Inj (SUBLIMAZE) (mcg) Total dose: 75 mcg
11/26/25 0805 50 mcg Given intraVENOUS Valdes, Luis E, RN
0810 25 mcg Given intraVENOUS Valdes, Luis E, RN
Midazolam Inj (VERSET) (mg) Total dose: 1.5 mg
11/26/25 0805 1 mg Given intraVENOUS Valdes, Luis E, RN
0810 0.5 mg Given intraVENOUS Valdes, Luis E, RN
Lidocaine (PF) 10 mg/mL (1 %) Inj (XYLOCAINE) (mg) Total dose: 40 mg
11/26/25 0809 40 mg Given Subcutaneous Vimr, Ross Patrick, MD
nitroglycerin in D5W 100 mcg/mL injection solution (mcg) Total dose: 200 mcg
11/26/25 0811 100 mcg Given intr-arterial Vimr, Ross Patrick, MD
0827 100 mcg Given intr-arterial Vimr, Ross Patrick, MD
Verapamil Inj (ISOPTIN) (mg) Total dose: 1 mg
11/26/25 0811 1 mg Given intr-arterial Vimr, Ross Patrick, MD
heparin (porcine) Inj (Units) Total dose: 3,000 Units
11/26/25 0812 3000 units Given intraVENOUS Valdes, Luis E, RN
iohexoL Inj (OMNIPAQUE 300) (mL) Total volume: 40 mL
11/26/25 0828 40 mL Given injection Vimr, Ross Patrick, MD
bacteriostatic sodium chloride 0.9 % Inj 0.2 mL (mL) Total dose: Cannot be calculated* Dosing weight: 77.6
Sodium Chloride 0.9% injection solution syringe 3 mL (NORMAL SALINE FLUSH) (mL) Total dose: Cannot be
Olga's comments:
Right dominant coronary arteries with single vessel obstructive CAD manifested as a long, chronic occlusion in the mid LAD LVEDP 10mmHg Deflate TR band per protocol Continue optimal medical therapy Will discuss revasc options with patient. Stenting is probably feasible but would require ~80mm of stent and thus not be expected to be a durable option
What I remember from the discussion. The 99% occluded part is about 84mm long and would have required two of their longest stents. The occlusion was so bad that the chance of successful stenting was low and it would not be a durable fix --- expected lifetime less than 5 years.
Time to schedule bypass surgery!
Meet my cardiothorasic surgeon, Dr. Isidore Dinga Madou, MD
 The day after Thanksgiving, I
got a call from Cardiothoracic surgury scheduling and an
appointment to meet with a surgeon next Tuesday at 2:30pm.
The doc was getting out of surgery late, so my appointment
was postponed a couple of hours, but no problem for me. I
was doing a lot of thinking!
The day after Thanksgiving, I
got a call from Cardiothoracic surgury scheduling and an
appointment to meet with a surgeon next Tuesday at 2:30pm.
The doc was getting out of surgery late, so my appointment
was postponed a couple of hours, but no problem for me. I
was doing a lot of thinking!

When Dr. Isidore Dinga walked in, I was surprised to see an African man wearing a Kufi cap. He was calm, had a firm handshake, and spoke confidently answering all of my questions. He said there's a chance they could do the surgery off-pump on the beating heart, and if they can do that, it greatly eases the recovery as the lungs are not collapsed and the body is not chilled. Also, he would try to use my left radial artery indstead of taking a vein from my leg. The artery is more robust lasting typically about 25 years. And as long as I didn't play guitar or need a lot of dexterity from my left hand, the impact would be small. Also, while it would be good to do the surgery soon, he was booked until February. However, he had a cancellation next week Tuesday (one week from now) and I could have that slot if I wanted it.
I took the slot.
I then had an hour or so of informational meetings with nurses who explained things and loaded me with packets of information. I got an Insentive Spirometer to exercise my lungs, got a list of tests that would have to be completed over the next few days, and was sent on my way at 7pm, just after the blood testing lab closed. I would be back several times before checking in for the surgery on Tuesday morning at 5:45am.
More about Dr. Dinga
I was born in Pointe-Noire, the economic capital of the Republic of the Congo, in central Africa. I moved to the United States in 2002 to learn English, then stayed and enrolled in college to study computer engineering at the State University of New York (SUNY) in Buffalo. My on-campus job was to create computer models of heart muscle ion channels to study the effect of different drug concentrations on heart muscle electrical activity, which led to my being exposed to cardiac surgery my last month of college. I found myself in an operative room where a cardiac surgeon was performing an aortic valve replacement (AVR) and Coronary Artery Bypass Grafting (CABG). Right there, as I watched from the side, it was like love at first site. I did not know what the surgeon was doing or how he was doing it, but I knew that this was what I had been looking for and that I was going to dedicate myself to it for the rest of my life. Being a heart surgeon is not my job but my vocation. I am humbled and blessed with an opportunity to make a difference in a fellow human life every day that I am at work. This is also a responsibility that I do not take lightly.
I joined the Department of Cardiothoracic Surgery at Kaiser Permanente Northwest because its patient-care philosophy resonates well with my core values. We are a patient-centered multidisciplinary team dedicated to treating each person based on their individual needs. We want to add value to the life of our patients, not take away from them. I have a personal interest in treating aortic and structural heart valvular diseases, but my practice incorporates all aspects of adult cardiac surgery with conventional open, minimally invasive, transcatheter, and endovascular techniques to surgically treat cardiovascular diseases.
Back home, we say that it takes a village to raise a child. Well, the same thing is true about cardiac surgery. It takes a village to get someone through an open-heart surgery. I can’t do what I do without a dedicated team of men and women who are passionate about what they do. I am always amazed by the care that they provide every day, not only to our patients but also to one another. I am honored and humbled to work alongside this smart, dedicated, devoted, committed, passionate, fun, caring, and compassionate group of individuals — who always advocate for our patients. I love the fact that we treat our patients and each other like family.
The whirlwind of tests begins (blood labs)
 Since I just missed getting my blood drawn on the way out of my Dr. Dinga meeting, I dropped into Kaiser
Cascade the next day for yet another EKG, blood draw, and urine test.
Since I just missed getting my blood drawn on the way out of my Dr. Dinga meeting, I dropped into Kaiser
Cascade the next day for yet another EKG, blood draw, and urine test.
CAT Scan (Longview)
 Then the next day I drove an hour north to Longview for a Cardiac CAT scan. The machine is pretty cool
with a thing that spins around your body as you lay on a table which slides through the core. Elapsed time for 3 scans about 15 seconds.
Then the next day I drove an hour north to Longview for a Cardiac CAT scan. The machine is pretty cool
with a thing that spins around your body as you lay on a table which slides through the core. Elapsed time for 3 scans about 15 seconds.
Leg Vein Mapping Ultrasound (Sunnyside)
 The next afternoon (Saturday), I drove back south to Sunnyside for a vein scan ultrasound to map out
the veins they might use for the bypass graft. They only scanned my legs which unnerved me as I distinctly remember Dr. Dinga saying
he prefers to use the left radial artery. I asked them to scan my arm too just to be sure, but they refused. Turns out the surgical
team has their own ultrasound in the operating room and didn't need the leg data. Yay!
The next afternoon (Saturday), I drove back south to Sunnyside for a vein scan ultrasound to map out
the veins they might use for the bypass graft. They only scanned my legs which unnerved me as I distinctly remember Dr. Dinga saying
he prefers to use the left radial artery. I asked them to scan my arm too just to be sure, but they refused. Turns out the surgical
team has their own ultrasound in the operating room and didn't need the leg data. Yay!
US EXTREM VEIN MAPPING, LIMITED (US DUPLEX SCAN EXTREM VEIN, LTD) - Final result (12/06/2025 3:36 PM PST) Anatomical Region Laterality Modality Leg, Arm, Foot, Ankle, Shoulder, Hand, Elbow, Finger, Fingers Ultrasound Specimen (Source) Anatomical Location / Laterality Collection Method / Volume Collection Time Received Time 12/08/2025 8:22 AM PST Usable length of greater saphenous veins: Right 51 cm. Left 50 cm. Electronically signed by Kevin C Lacour, MD. 12/8/2025 8:23 AM Results - US EXTREM VEIN MAPPING, LIMITED (US DUPLEX SCAN EXTREM VEIN, LTD) - Final result (12/06/2025 3:36 PM PST) Narrative 12/08/2025 8:23 AM PST This result has an attachment that is not available. EXAM: US DUPLEX SCAN EXTREM VEIN, LTD EXAM DATE AND TIME: 12/6/2025 3:15 PM HISTORY: US EXT VEIN MAPPING UNILATERAL OR LIMITED BILATERAL Date of Surgery: 12/9/2025; Type of Surgery: CABG. Which Vein: GSV Bilateral TECHNIQUE: Multiple transverse and longitudinal grey scale images of the lower extremity superficial veins were obtained. FINDINGS: Side Imaged: Right Vessel Imaged: Greater saphenous vein Measurements (millimeters) perforators/branches: Groin: 3.8 Proximal thigh: 3.7 Mid thigh: 3.1 Distal thigh: 3.2 Knee: 3.4 Proximal Calf: 3.0 Mid calf: 2.7 Distal calf: 2.4 Ankle: 3.5 Length of Usable Segment: 51 Side Imaged: Left Vessel Imaged: Greater saphenous vein Measurements (millimeters) perforators/branches: Groin: 3.8 Proximal thigh: 3.1 Mid thigh: 3.2 Distal thigh: 3.8 Knee: 3.7 Proximal Calf: 3.8 Mid Calf: 2.9 Distal Calf: 2.3 Ankle: 3.2 Length of Usable Segment: 50 IMPRESSION: Usable length of greater saphenous veins: Right 51 cm. Left 50 cm. Electronically signed by Kevin C Lacour, MD. 12/8/2025 8:23 AM
Blood type and cross-check (Cascade)
 Within 48 hours of surgery, they
need blood type and "cross match" which is a check of
various antibodies. Choosing blood for transfusions these
days is a lot more complicated and they really hate to use
foreign blood if they can avoid it. I had asked about
pre-donating my own blood, but it takes about a month to
recover from a blood donation and they really aren't
equipped to store special blood for special patients.
Turns out they didn't need to add any foreign blood. "Vac
it up, Filter it, Spin it, and shove it back in," one of
the nurses told me. Cool! But it does leave you anemic with
low RBC, Hemoglobin and low Hematocrit. That all takes about a
month to recover and I think it's part of the whole being-tired-after-surgery experience.
Within 48 hours of surgery, they
need blood type and "cross match" which is a check of
various antibodies. Choosing blood for transfusions these
days is a lot more complicated and they really hate to use
foreign blood if they can avoid it. I had asked about
pre-donating my own blood, but it takes about a month to
recover from a blood donation and they really aren't
equipped to store special blood for special patients.
Turns out they didn't need to add any foreign blood. "Vac
it up, Filter it, Spin it, and shove it back in," one of
the nurses told me. Cool! But it does leave you anemic with
low RBC, Hemoglobin and low Hematocrit. That all takes about a
month to recover and I think it's part of the whole being-tired-after-surgery experience.
ABORH TYPE ANTIBODY SCREEN PROFILE (FOR CROSSMATCH) (TYPE AND SCREEN FOR CROSSMATCH) Result (12/07/2025 2:04 PM PST) Component Value Ref Range Test Method Analysis Time Performed At Pathologist Signature ABO Type A Rh Type Negative Antibody Screen Negative

cooking some chicken soup for the freezer and post-surgery recovery.
Day 0: The Surgery
 On the day of the surgery, I
got up at 3:00am to drink my 6oz of clear carbohydrate
drink, then up again at 4:15am, took the last of my 4 days
of twice-a-day showers with Hibiclens antibactieral soap,
patting dry with a freshly washed towel, took my statin and
vasodilator but not my aspirin, then jumped in the car to
drive myself south to Sunnyside in a torrential rainstorm. I
had three significant hydroplaning episodes on the way and
was glad to make it there in one piece.
On the day of the surgery, I
got up at 3:00am to drink my 6oz of clear carbohydrate
drink, then up again at 4:15am, took the last of my 4 days
of twice-a-day showers with Hibiclens antibactieral soap,
patting dry with a freshly washed towel, took my statin and
vasodilator but not my aspirin, then jumped in the car to
drive myself south to Sunnyside in a torrential rainstorm. I
had three significant hydroplaning episodes on the way and
was glad to make it there in one piece.

Hey KB, this is where I parked the car!
I was supposed to be there at 5:15am, but I was about 15 minutes early, so I had to wait for reception to open.
Then, down the hall, pick up the phone to let them know I was there. I was whisked in immediately to be weighed, undressed, shaved, two IV lines inserted into my right hand and right wrist.
Ann (Anesthesia) Stevens was my anesthesiologist assisted by her resident Dr. Ming. It was nice to see her familiar face and super calm and reassuring demeanor. Then I had a visit from Whiteny the PA leading the arm surgery team who was going to take my radial artery --- such a relief about the whole leg vein scan thing. Finally Dr. Dinga arrived and held my hand as they wheeled me into the OR.
The room was filled with about 10 people who would be working on me. Dr. Dinga knelt down beside my bed and took my left hand in his two, very warm hands. In a soft voice, he said, "Team, this is Chris Uhlik and it is my pleasure that we will fix him up today. Please, everyone introduce yourselves and tell Chris what is is you are going to do. I remember a very diverse group of skilled professionals recite their names and a brief summary of their work, then the room went fuzzy, and ....
TRANSESOPHAGEAL ECHO, ANESTH PROC (Anesthesia TEE) - Final result (12/09/2025 7:42 AM PST) Stevens, Ann Elizabeth, MD 12/9/2025 11:43 AM Anesthesia TEE Patient location: OR Indications: Perioperative monitoring Time out: Pt ID verified with 2 separate identifiers, Procedure verified, Consent obtained, Side verified and marked as appropriate, Time out performed immediately prior to start of procedure Placed at: Post-induction Start time: 12/9/2025 7:42 AM Surgeon requested TEE: Yes Color flow and doppler: Yes Probe insertion: Easy Quality of study: Optimal Left Ventricle Cavity size: Normal Hypertrophy: Yes Hypertrophy yes: Mild Thrombus: No Global function: Normal LVEF%: 50-55 Wall motion abnormality: None Right Ventricle Cavity size: Dilated Cavity size dilated: Moderate Hypertrophy: No Thrombus: No Global function: Mildly depressed Ventricular septum: Normal Left Atrium Size: Normal SEC (smoke): No Thrombus: No Tumor: No Device: No Atrial appendage: Normal Right Atrium Size: Dilated SEC (smoke): No Thrombus: No Tumor: No Device: No Atrial septum: Normal Aortic Valve Annulus: Normal Stenosis: None Regurgitation: None Leaflet morphology: Normal Leaflet motion: Normal Mitral Valve Annulus: Normal Stenosis: None Regurgitation: Trace Pulmonic vein wave: S
 onwards to the post surgery, recovery experience.
onwards to the post surgery, recovery experience.






