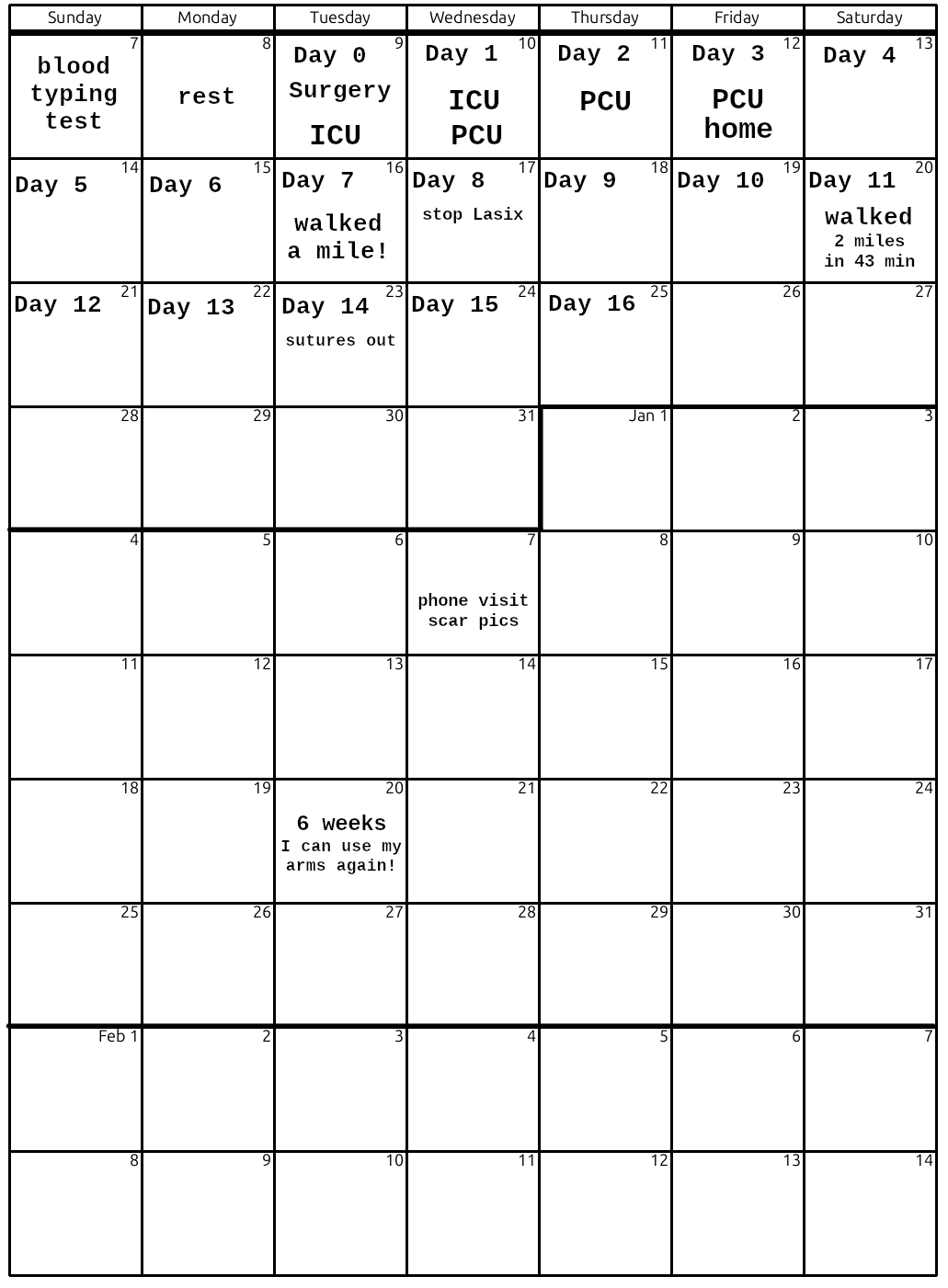
Waking up in the ICU
 I remember holding Kathi's hand as I was waking up. I don't know how long it took to regain consciousness.
According to the surgical log, I went in at 7:42am and was out around 12:30pm.
I remember holding Kathi's hand as I was waking up. I don't know how long it took to regain consciousness.
According to the surgical log, I went in at 7:42am and was out around 12:30pm.

These are the nine drug pumps metering special sauce back into my jugular vein.

This is the remote monitor connected to a box wired into me via WiFi. Continuous arterial blood pressure, SpO2, and an EKG.

Rosalie was my 1-on-1 ICU nurse for the waking up period. Here she is using a small ultrasound machine to measure blood flow into my hand.
She performed dozens of tests and monitored me very closely.
That's the arm from which they removed the radial artery.

This is my heart pillow which I am to hug to my chest to relieve pain and avoid using my arms and stressing my new sternum joint.
A big goal for later today is to get me up and into that chair.

Joci and Vivi visited me along with Kathi.
Vivi is staying out of the room to minimize any chance of infection.

Helping Chris out of bed at 5:30pm

The things on my legs are pressure cuffs which help keep blood from pooling in my lower extremities.

Dr. Dinga stopped by at 5:47pm to witness Chris sitting up!

I have to say, the last thing I wanted to see was that Insentive Spirometer. I think I hit maybe 300 out of 2500.

I'm soooo thirsty! But I'm also on a strict fluid limit as I've got 4 extra liters of fluid in me from all the IVs. They really don't want me drinking anything until my kidneys wake up. I'm on a Foley Catheter, so I don't have to worry about peeing.

I've got a main line into my jugular vein so they can dump drugs directly into my heart if necessary.

I am so fortunate to have a personal recovery angel!

Michelle sent flowers, but they aren't allowed in the ICU.

Flower colors were chosen by Deborah and Michelle to appeal to a Red-Green colorblind guy like me! Nice touch.
Day 1: Transfer to the PCU
 The big goal for today is to
eat, get some sleep, and get up to walk 4 times, at least 50
feet. If I can do all that, they can transfer me from
Intensive Care (ICU) to Progressive Care (PCU) where I'll be
under the supervision of a nurse that is watching 2 or 3
patients rather than 1-on-1. I'm feeling pretty good. I
let the nurses put me on pain meds which was a good choice
as with-meds I can me breath almost normally.
The big goal for today is to
eat, get some sleep, and get up to walk 4 times, at least 50
feet. If I can do all that, they can transfer me from
Intensive Care (ICU) to Progressive Care (PCU) where I'll be
under the supervision of a nurse that is watching 2 or 3
patients rather than 1-on-1. I'm feeling pretty good. I
let the nurses put me on pain meds which was a good choice
as with-meds I can me breath almost normally.

That orange stuff in my beard is the
betadine-like stuff they paint you with for a sterile field. My eyes are also greasy from whatever they lubricated them with in surgery (glycerine, vasoline?)

These nurses know how to bring a guy back from the dead; COFFEE!!!

7:24am, I didn't sleep much last night, but I'm feeling pretty fine jacked up on fentaynl and oxycodone and that wonderful cup of coffee

They are getting me up to walk out into the hall, then back to my chair, goal >20ft.

I'm not exactly hungry, but I eat all the food: oatmeal, banana, yoghurt. I eat really slowly, but keep everything down. Great progress. 2pm

Here is an example of some of the continuous testing that is going on. I'm on an insulin pump and they are coming in to collect blood every hour to hold my blood sugar in the ideal range for healing.

3:30pm out for another walk, this time it's a long one, all the way to the PCU. I didn't quite make it, but they had the wheelie chair to catch me at the end when I ran out of gas.

3:30pm, Walking to my new room in the PCU

I still have all my drain tubes in.

This is Dylan, my wonderful PCU support nurse during the day.

My left arm is bandaged from the artery removal. I have a transmitting EKG and blood gas monitor in my pocket. Hanging on the walker is the backup pacemaker (black) and three measuring drain boxes for the two chest tubes and the Foley catheter.

Salmon protein slab with green beans.

Crushing the walking goals. TBD: Bowell Movement, Care Giver Training, learn how to Take a Shower.

Trying to update friends without scaring the shit out of them.
That left arm works to hold a phone as long as I don't try to rotate the forearm or bend the wrist.
Day 2: PCU, getting tubes out, and walking
 Today's goals, walk 4 times,
visit the toilet, get the chest drain tubes out, get the backup
pacemaker wires out, get the Foley Catheter out, get the main line out
of my neck, etc.
Today's goals, walk 4 times,
visit the toilet, get the chest drain tubes out, get the backup
pacemaker wires out, get the Foley Catheter out, get the main line out
of my neck, etc.

4:30am, they sat me up to shove an X-Ray panel behind my back.
The nurse begrudgingly let me take a picture of the screen. You can see the wires holding my sternum together, all the EKG
leads, and the backup pacemaker wires laying on my heart. Their primary interest is to make sure my lungs aren't collapsing.

Exhausted selfie. 7:30am after my second night of being awakened every hour for blood tests, chest X-rays, 12-lead EKG placement, etc. You don't get to sleep much.

8:37am after breakfast of scrambled egg substitute (uggh!) and oatmeal. My hunger isn't normal, but it's not so weird that I can't force myself to eat the food.
Taking out one of the chest tubes
My nurse PA Nathan AKA "Big Nate" came in and removed one of my chest drain tubes and my backup pacemaker around 10:00am. The drain tube lets excess pleural fluid (a type of serous fluid, pale yellow, transparent fluid, which acts as a lubricant) around the lungs drain. Normally this fluid is produced and reabsorbed at a rate of about 20 mL/day, but the surgeons irritated everything so I'm making the stuff much faster than normal for a couple of days. When the drain rate falls enough, they pull out the tubes.
Yesterday, they tested my backup pacemaker. That was really interesting. The purpose of the backup is to prevent my heart rate from falling too low. For most of my stay, my heart rate has been about 100 bpm and they don't want it falling below 80. For the test, they raised the threshold to my heart rate, watched the machine lock phase, and then raised the rate a bit more. I could feel my heart rate follow the knob on the machine. It seemed very natural, my heart just sped up. Then they eased it back down and the machine let go. Comforting.
Pulling out the backup pacemaker wires was an extremely weird sensation. Nate did it quickly, all in about 2 seconds. But it felt like he had reached into my chest, grabbed a nerve in my arm, and yanked it out. The sensation started at my finger tips and stimulated everything inside me. Electric and unpleasant, but brief and not too painful.
Pulling out the chest tube was also quick and not quite as weird, but more painful. "Take a big breath and bear down," said Big Nate. The pulling was over in a second, but the pressure on the opening and tightening up the suture lasted maybe 20 or 30 seconds.
Somewhere in there, they also pulled the main IV line from the jugular vein in my neck and removed the Foley Catheter. Using a toilet is easier than I expected. My legs are still strong, but I do need assistance getting out of the bed.

There it is after the pacemaker wires and one chest tube have been
removed. I'm still bloated from the excess IV fluids. My urine
production is about 100 mL/hr and they are putting about 30 mL/hr
into me with all those drug pumps, and I am drinking a little bit
and getting fluid from my food intake, so maybe 2400 mL/day out and
2000 mL/day in, getting rid of 4 liters is going to take a few days.

Relieved and breathing a little easier.

Out for a walk with Nurse Jane. Getting
up is easier with only one drain box and no backup pacemaker to deal with. I'm doing laps around the PCU floor, roughly 800 ft per lap I estimate. Dr. Dinga told the nurses, "Let him walk as much as he can. He is not restricted in number of walks or distance. If he can do 2 miles, let him do 2 miles."
Taking out the other chest tube
I stayed in bed for an hour as instructed after getting the first chest tube out. But then, while standing up to go for a walk the other chest tube's blood clot let go and I dumbed some blood and fluids on the floor. This caused a minor emergency where they decided to pull the second tube and install a compression dressing just below my sternum. Another hour laying still in bed for that to set up before I can go walk. But wow! I can really breath so much easier with no tubes passing between my diaphram and my ribs.

Feeling well enough to tap out a few messages to a few friends. Getting your well wishes was really spirit lifting, but trying to reply was exhausting. So appologies if you sent me your wishes and I didn't respond. I really, really did appreciate your thoughts!

Tony stopped by on his way home from work Thursday night at about 8pm. We got to talk for an hour and he took me around the floor for a few laps. I'm feeling like I might be able to go home tomorrow.
Release from PCU to Home Care

The dressing was removed from my arm this morning. They used 8 inches 200mm of radial artery. The careful removal of that artery is a pretty major surgery as well. They were in my arm for about 90 minutes from incision to close.
Caregiver Training
Kathi came in for CGT CareGiver Training at 10:00am. We learned about washing incisions, use of the chest binder, use of the spirometer, what foods to eat and not eat, sleeping in a recliner chair, not using arms, being really careful to avoid using arms reflexively, how to ride in a car, under what circumstances to get back to the hospital, etc. Lots of really practical stuff given in a tone quite different to the "don't sue us" written materials.


My super PCU nurses Jane and Dylan -- you guys really made it easy to recover quickly in the PCU!

12:15pm, Chris dressed up in outside clothes and itchin' to be outta here!

Getting instructions about all my new meds.
The ride home
Kathi and I stoped to pick up Poke bowls across the street, then I ate lunch while Kathi drove very carefully in heavy traffic. I didn't stay conscious for long. I fell asleep and woke up in the garage at home feeling pretty wasted.

Recovering from the ride home on the couch with my big bag of meds.

Figuring out all the stuff I have to take now.

There it is all organized for the next 2 weeks so I don't have to think in the middle of the night.

My hand is strong but the range of motion of my wrist and forearm is sharply limited for now. Nicky gave me this fidget ball thing to keep my hand busy. Works great!
It's so good to be home. I had a really awesome night sleep where nobody stabbed me even once in the night!
Day 4 Continuing Recovery at Home, Saturday Dec 13

Starting to write up this experience.
I can stand for about an hour before I run out of energy.

I took a shower but this dressing isn't drying like I think it should. I called the advice line and learned it should have been removed before sending me home. It came off pretty easily after being soaked in the shower.

Before and after pics for the advice nurse.
The two holes with sutures are where the drain lines were placed. The wound near my belly button is where the backup pacemaker wires entered. That scar is going to be something else for a while!

Maybe I should get it decorated something like this... hmmmm...

28 care team notes documents that Kaiser doesn't let me download, but on my computer I can drag across the HTML and copy text. They don't let it print either and I don't feel up to hacking the javascript to override their restrictions.
Day 5 Continuing Recovery at Home, Sunday Dec 14


Here are the meds I take every morning.

Incisions are healing well and I've lost about 4 of the 10 lbs I gained during surgery.

This powered air pad thing on the chair
is awesome. It has ~130 air baldders inside and a very quiet air pump. On a 20 minute cycle, it deflates one set and inflates another relieving pressure points. This makes it possible for me to sleep on my back in one position all night long. I'm getting really good sleep as long as I stay on Tylenol. I wake up twice each night, use the powered chair to get up, go pee, walk around, take another Tylenol, then right back to sleep. So far, I haven't used any oxycodone, just Tylenol about 325 or 500 mg every 3 to 6 hours.
Day 6 Continuing Recovery at Home, Monday Dec 15

I baked sourdough bread today. I let the mixer do all the kneeding work. To keep the saturated fat low, I use olive oil instead of butter. And to keep the sodium low, there's only 3/4 tsp of salt in the bread, and I use a salt shaker to add a little salt to the olive oil on the bread. Heavenly! I hope it promotes healing as much as it tastes like it!
Day 7 Continuing Recovery at Home, Tuesday Dec 16 (one week after surgery)
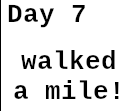 Today I walked a mile.
Today I walked a mile.

I walked to the end of this vacant lot. Rested a bit. Then walked back home. I thought the total was about a mile, but I guess it's more like 0.8 miles. Anyway, this is a big milestone for me. It's very near my aerobic limit right now. It sure beats sitting on the couch working the Incentive Spirometer.

Going through the *MANY* test reports, I came across this Chext X-Ray Report from post-surgery Day 2 (the day before my release to home care).
Let's see if Gemini can help translate it into simple English...
| Report Line | Explanation |
|---|---|
| Median sternotomy wires are redemonstrated. | This is normal and expected. It means the surgical team used wires to close and secure the breastbone (sternum) after the surgery. "Redemonstrated" just means they can clearly see the wires, confirming the surgical closure is intact. |
| The left-sided chest tube has been removed. | The chest tube is placed during surgery to drain blood and fluid from around the heart and lungs. Its removal is a positive step, indicating the surgeon felt the immediate major bleeding/fluid accumulation risk was low enough to take it out. |
| There is no pneumothorax. | This is excellent news. A pneumothorax is a collapsed lung, where air leaks into the space between the lung and the chest wall. The X-ray confirms your lungs are fully inflated. |
| Stable mediastinal contours. | The "mediastinum" is the central compartment of your chest containing your heart, major blood vessels, and windpipe. "Stable contours" means the size and shape of these organs, especially the heart, have not changed or shifted, and there are no signs of abnormal swelling or bleeding around the heart (like a hematoma). |
| No pulmonary vascular congestion. | This is another very good sign. It means there is no buildup of fluid in the blood vessels of your lungs. This finding suggests your heart is pumping effectively and not failing to clear blood from the lungs. |
The Last Sentence: Trace Left Pleural Effusion and Left Basilar Opacity which likely reflects atelectasis.
This is the most technical part, but it is a very common and generally minor finding after heart or chest surgery.
- Trace Left Pleural Effusion:
Pleural Effusion is fluid collecting in the pleural space (the thin space between the lung and the chest wall).
- "Trace" means it is a very small amount. This is expected after surgery, as some inflammation and fluid leakage are normal parts of the healing process.
- "Trace" means it is a very small amount. This is expected after surgery, as some inflammation and fluid leakage are normal parts of the healing process.
- Left Basilar Opacity:
- "Opacity" just means an area on the X-ray that looks white or hazy (it's not clear or black like normal air-filled lung tissue).
"Basilar" means it's at the base (bottom) of the left lung.
... which likely reflects atelectasis.
- "Opacity" just means an area on the X-ray that looks white or hazy (it's not clear or black like normal air-filled lung tissue).
- "Atelectasis" is the technical term for a collapsed or deflated area of the lung.
It is sometimes called "splinting."
Why it happens: After major chest surgery, especially bypass, patients often breathe shallowly because of pain, being sedated during surgery, or having been lying on their back. The small airways and air sacs at the very bottom of the lung don't fully inflate, causing a small, temporary collapse or deflation.
Significance: It is not usually a major complication and is managed with post-operative care, such as encouraging deep breathing, coughing, and using an incentive spirometer.
In summary, the last sentence means you have a tiny bit of fluid around your left lung and a small, deflated area at the bottom of the left lung, both of which are common, expected, and usually treatable effects of the recent surgery.
In simple terms, the X-ray was good: The wires are in place, the heart area looks stable, your lungs aren't collapsed, your heart isn't backing up fluid into your lungs, and the only abnormal findings (a little fluid and a tiny deflated lung spot) are minor and expected after bypass surgery.
Would you like me to find some information on how to use an incentive spirometer, which is often prescribed to help with atelectasis?
Aside: Gemini 2.5 Fast is frickin' amazing! AI is going to revolutionize health care in 2026 if the government doesn't fuck it up, which I'm sure they will make every effort to do. I hope it remains available in single-payer-healthcare countries and I can get at it via VPN.
Well that read of the X-Ray report is so good to know! This interpretation strongly encourages me to work harder with my Spirometer and to get out and walk more. I need to get that lung completely reinflated. I guess this is part of why I'm so short of breath. Another explanation is my anemia. While I didn't "lose a lot of blood" during the surgery, they did vac, spin, filter, and put a significant about of my blood back in which removes red blood cells. My RBC and hematocrit and hemoglobin are quite low and they tell me that takes a month to fully recover. Thus the FerroSul and Ascorbic Acid supplements to aid iron absorption.
Day 8 Continuing Recovery at Home, Wednesday Dec 17
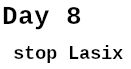 my weight has been dropping steadily about 1--1.5 lbs per day. Today I passed below my ideal pre-surgury weight
and I'm feeling a bit dehydrated. I cut my morning Lasix and corresponding potassium support in half and sent a message to the advice nurse. I tried to leave a message with Cardiology two days ago, but they have not answered yet. Today, I'm taking this into my own hands and going to wait on the advice line until I talk to someone. No more leaving messages! After I got through, I waited 4 hours for a call back, and Heather told me to stop the Lasix and ordered a set of blood labs. Kathi drove me into Cascade for a blood draw and EKG.
my weight has been dropping steadily about 1--1.5 lbs per day. Today I passed below my ideal pre-surgury weight
and I'm feeling a bit dehydrated. I cut my morning Lasix and corresponding potassium support in half and sent a message to the advice nurse. I tried to leave a message with Cardiology two days ago, but they have not answered yet. Today, I'm taking this into my own hands and going to wait on the advice line until I talk to someone. No more leaving messages! After I got through, I waited 4 hours for a call back, and Heather told me to stop the Lasix and ordered a set of blood labs. Kathi drove me into Cascade for a blood draw and EKG.
Day 9 Continuing Recovery at Home, Thursday Dec 18

Feeling damn good this morning!
I got my blood lab results back.

These show my kidneys are working hard to get rid of all the excess nitrogen from my 100g-protein/day diet.

And these are the side effects of removing so many of my red blood cells during surgery.

Nurse agrees with my call to stop the diuretic and drink a little more.
Day 10 Continuing Recovery at Home, Friday Dec 19 a longer walk

 >
>
I walked down the lawn to the river in the rain to see the high water. It's almost up on the grass, maybe 8ft higher than usual. We are having a lot of rain.


As I was walking in light rain, almost a half mile from home, the sky opened up with a hailstorm (~3mm ice balls).

But it didn't last long, and I got a little bit of rainbow reward.

Pushing a little farther down the street, now it's an honest mile, plus.
Day 11 Continuing Recovery at Home, Saturday Dec 20
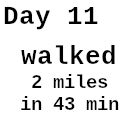 Today I walked all the way to the end of Rivershore drive. I love that every day I see progress without the rollercoaster they warned me about. As long as I don't get an infection, I am feeling better and better every day!
Today I walked all the way to the end of Rivershore drive. I love that every day I see progress without the rollercoaster they warned me about. As long as I don't get an infection, I am feeling better and better every day!

21m out and 23m back. It was a pretty big effort, but I feel a great sense of accomplishment.

Got a nice present from Lizzie's mom. It's a special pillow to protect my chest from car shoulder belts. Nice, mmmmm!
Day 12 Continuing Recovery at Home, Sunday Dec 21
Day 13 Continuing Recovery at Home, Monday Dec 22
Walked 2 miles, then went out later in the day and did another 2 miles.
Blood Testing, especially Lipid Panel Results
I often see these nominal ranges quoted
| Cholesterol | ||||
| desirable | <200 mg/dL | |||
| borderline | 200-239 mg/dL | |||
| high risk | >239 mg/dL | |||
| Triclyceride | ||||
| desirable | <499 mg/dL | |||
| borderline | ≥500 mg/dL | |||
| HDL | ||||
| desirable | >40 mg/dL | |||
| borderline | ≤39 mg/dL | |||
| LDL | ||||
| desirable | <159 mg/dL | |||
| borderline | ≥160 mg/dL | |||
| HbA1C | reflects average glucose levels over the past 3 months | |||
| ideal | ~4.6% | |||
| healthy | <5.7% | |||
| pre-diabetes | 5.7--6.4% | |||
| diabetes | >6.5% | |||
I was tested on 2020/12/10, 2024/12/19, again on 2025/10/02, then Dr. Demina put me on rosovostatin and I was tested again, two months later before surgery on 2025/12/04.
| Cholesterol | 191 | 206 | 201 | 168 | borderline, Down 16% to desirable, still not great |
| Triglycerides | 61 | 38 | 102 | 70 | desirable, down 31% from 102 |
| LDL | 116 | 132 | 123 | 91 | desirable, down 31% from 123 |
| HDL | 60 | 66 | 58 | 63 | desirable, statins don't improve this |
| HbA1C | 5.4% | 5.7% | N/A | N/A | borderline pre-diabetes, not great |
| ApoB | 91 | N/A | N/A | N/A | not <90, so not great |
| Lp(a) | 41 nmol/L | N/A | N/A | N/A | <75, so good genetics; then why me? |
However, consider that Dr. Peter Attia considers these "dangerously lenient" because they reflect what is "normal" for a population where heart disease is the leading cause of death. Hmmm.
Attia considers ApoB (The Gold Standard Test)
Attia considers Apolipoprotein B (ApoB) the single most important metric. ApoB measures the total number of
"bad" particles (LDL, VLDL, and IDL) that can get trapped in artery walls and cause plaque.
Optimal: Stay Below 60 mg/dL (only 5% of the population achieve this).
Attia says that if everyone’s ApoB was between 20–30 mg/dL
starting in their 20s, atherosclerotic heart disease would be virtually eliminated.
Standard Lab "Normal": is <90 or <100 mg/dL, but Attia considers this far too high --- in 2020 I measured 91. It was probably already too late, but I should have gone on statins then.
LDL-C Low-Density Lipoprotein (A Noisy Surrogate)
Attia views LDL-C as a "noisy surrogate." Since one
ApoB molecule exists on every LDL particle, measuring the
particle count (ApoB) is more precise than measuring the
mass of cholesterol inside them (LDL-C).
Attia’s Target: He doesn't focus on a specific LDL-C
number as much as ApoB, but generally, an LDL-C <30
mg/dL correlates with the extremely low risk seen in
those with the 20–30 mg/dL ApoB target.
Note that even on the statin CRESTOR, I'm at 91 mg/dL which is way above (300% of) Attia's target of <30.
Triglycerides & HDL-C (The Metabolic Ratio)
Instead of looking at HDL-C ("good cholesterol") in isolation, Attia focuses on the
Triglyceride-to-HDL ratio as a proxy for insulin sensitivity and metabolic health.
Ideal TG/HDL Ratio: <1:1 (e.g., Triglycerides of 50 and HDL of 60).
Acceptable Ratio: <2:1.
Triglycerides Target: <100 mg/dL is good, but <50 mg/dL is considered metabolically excellent.
HDL Note: Attia warns that very high HDL (over 80–100 mg/dL) is not necessarily "better" and can sometimes indicate dysfunctional HDL or genetic anomalies.
ApoA-I & The Ratio
Apolipoprotein A-I (ApoA-I) is the primary protein on HDL particles.
ApoB/ApoA-I Ratio: While this is a strong predictor of risk, Attia prefers to focus on lowering ApoB as the
primary lever, as raising ApoA-I (via HDL) has not been shown in trials to reduce heart disease risk as
effectively as lowering ApoB.
Lp(a) (Lipoprotein little-a)
This is a highly inflammatory, genetically determined particle.
Attia recommends everyone test this at least once in their life.
Optimal: <30 mg/dL (mass) or <75 nmol/L (particle count) --- I was 41 nmol/L in 2020, so good.
High Risk: Above 50 mg/dL or 125 nmol/L. If your Lp(a) is high, Attia argues you must be even more aggressive in
lowering your ApoB to compensate for this inherited risk.
VLDL Cholesterol
Very Low-Density Lipoprotein is a precursor to LDL and carries triglycerides.
Attia’s Target: <10 mg/dL.
Summary Table: Attia vs. Standard Lab Marker
| Marker | Standard target | Attia's target | Why? |
|---|---|---|---|
| ApoB | <90--100 | <60 mg/dL (Ideal 20-30) | Total count of all atherogenic particles. |
| LDL-C | <30 mg/dL | Correlates with the low ApoB leves seen in low risk populations | |
| Triclycerides | <150 | <50-75 mg/dL | Correlates wtih good fat metabolism |
| TD/HDL ratio | <3.0 | <1.0 mg/dL | A proxy for insulin sensitivity |
| Lp(a) | N/A | <30 mg/dL | Genetically determined; if high, you must lower ApoB even further |
| VLDL-C | <30 | <10 mg/dL |
Note: Attia frequently emphasizes that "cholesterol years" (the cumulative exposure of your arteries to ApoB over your lifetime) are what matter most. He advocates for aggressive management through diet (saturated fat reduction), exercise, and often pharmacology (statins, ezetimibe, or PCSK9 inhibitors) to maintain these low levels long-term.





























































